Pancreatic cancer results when abnormal cells in the pancreas grow exponentially and form a tumor. The pancreas has two types of cells, exocrine cells and endocrine cells, both with different functions. Most pancreatic cancers are considered to be exocrine tumors that start in the exocrine cells responsible for making the pancreatic enzymes that aid in digestion.
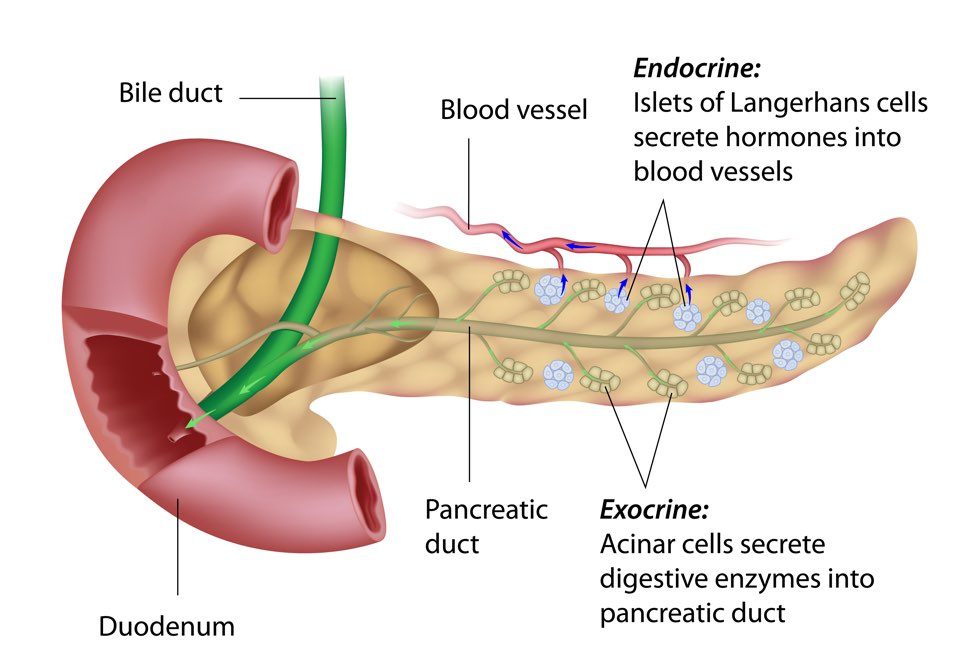
About 90% of these cases are considered to be adenocarcinoma and begin in the lining of the pancreatic duct. While there are a number of different exocrine tumors, when discussed this is typically the type of pancreatic cancer referred to, as it the most common and unfortunately one of the most aggressive.
Endocrine tumors, referred to as neuroendocrine tumors, are more rare and make up a round 5% of pancreatic tumors. These tumors develop from irregular growth of hormone producing endocrine cells called islet cells and can be both benign and malignant.
The slower growing tumors are often called “islet cell tumors” being a result of the islet cells overgrowing. There are two types of pancreatic neuroendocrine tumors, functional or nonfunctional.
Functional tumors cause the pancreas to overproduce and release hormones and often result in hormone-related symptoms.
While these symptoms may present sooner the majority of pancreatic neuroendocrine tumors are nonfunctional and do not have these symptoms so are found at a later stage.
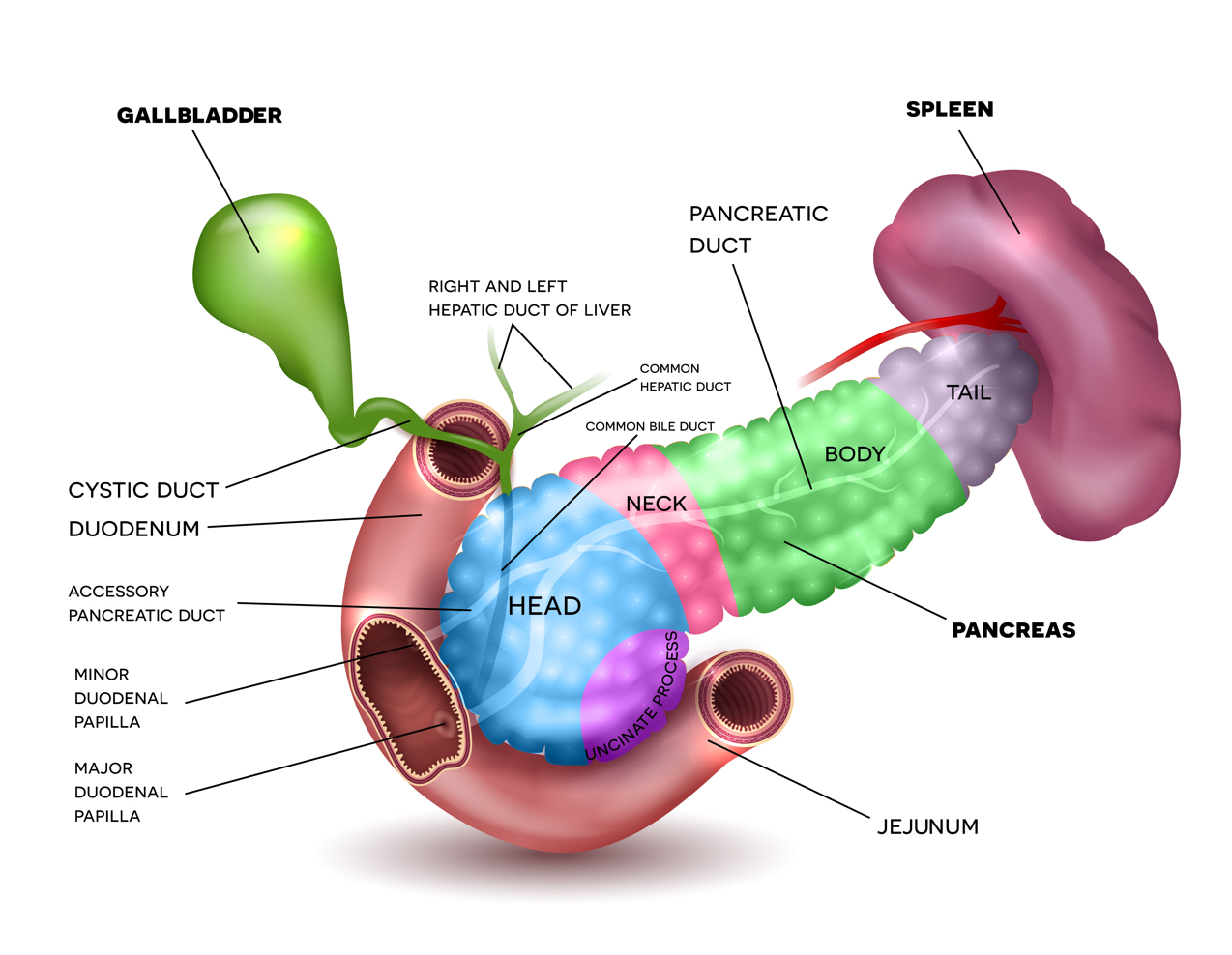
The pancreas is an approximately six inch long gland located in the abdomen. It is shaped like a long, flattened pear and located deep in the belly.
It is described in four parts: the wide end located on the right side of the body is the head, the middle sections are the neck and body, and finally the thin end that reaches the left side of the body is the tail. The pancreas borders the stomach, liver, spleen, gall bladder and small intestine.
Although the pancreas goes unnoticed in day-to-day life, it is a key part of the digestive system and is responsible for controlling our blood sugar.
The answer to this question is a difficult one, as the causes of pancreatic cancer are not fully understood.
While researchers continue to pinpoint a direct cause or link to pancreatic cancer they have found some risk factors that can increase the chances of developing pancreatic cancer. Individuals who have inherited a genetic mutation linked to pancreatic cancer, or with more than one immediate relative (parent, sibling, child) who has had pancreatic cancer, or one that developed the disease before the age of 50, are at a higher risk.
Other risk factors include: diabetes (risk increased with long-term, 5+ years) chronic pancreatitis (often linked to individuals with high alcohol consumption), smoking (smokers are 2x more likely to develop), race and ethnicity (people with African decent appear to have a higher risk over those with Asian, Hispanic, or Caucasian decent), age (chances increase with age, most being 60+), gender (small number of men more than women), diet (while still unclear, diets high in fruits and vegetables seem less likely) obesity (20% increased chance).
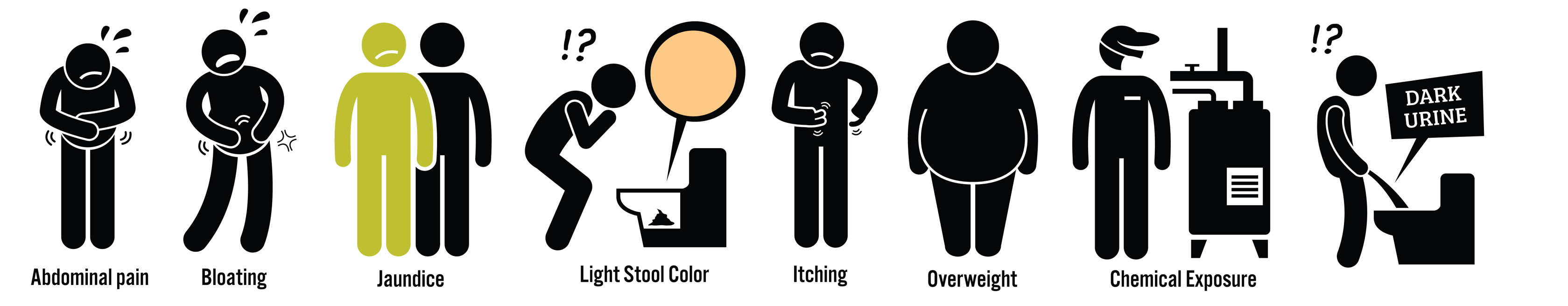
Pancreatic survival rates are immensely low and one main cause of this is late diagnosis. In most cases, pancreatic cancer symptoms are vague and mysterious and appear similar to much less serious and common problems. Early symptoms of pancreatic cancer can seem so subtle that they don’t raise concern or importance.
As a result of this, early detection is near impossible and awareness is currently the most successful tool available to early detection.
The most common symptoms of pancreatic cancer include: pain (in the upper abdomen or back), weight loss, jaundice (yellowing of the skin and eyes, sometimes itching), abdominal bloating, digestive problems (nausea, indigestion, loss of appetite), stool changes (discoloration, diarrhea, constipation, foul-smelling), blood clots, chronic pancreatitis and sudden–onset diabetes. (Note: if you are experiencing one or more of the symptoms please consult with your doctor)
Defining a patient’s qualification for surgery is difficult and even with advanced imagining it is often not clear as to what the tumor looks like. Generally a tumor in the pancreas is deemed resectable once it has not spread to other parts of the body or is not imposing on major arteries. Involvement of veins can cause hesitation however a qualified surgeon can complete the procedure.
The Whipple is the most common surgery used to remove pancreatic tumors, however it is a complicated operation lasting over 5 hours. It is usually performed if the cancer is in the head, neck or uncinate process of the pancreas. In a typical procedure the surgeon will remove the head of the pancreas, the gallbladder, the duodenum (the first part of the small intestine) and the bile duct. After performing this surgery the remaining organs are reconnected to allow for normal food digestion.
Distal Pancreatectomy is performed if the tumor is in the body or tail of the pancreas, the left side. Typically if a tumor is located in this area of the pancreas, symptoms develop slowly and are often undetected for some time, but if found this surgery can be performed. The surgeon will remove the body and tail of the pancreas and most often the spleen.
Total Pancreatectomy is performed when the tumor is located in such a way that the entire pancreas must be removed, or if there are multiple tumors in the pancreas. While life after this surgery is relatively normal the removal of the pancreas means that the patient will become diabetic and require insulin to control blood sugar levels as well as enzyme replacements.
Clinical trials are research studies that involve people and it is important to remember all approved drugs were at one point a clinical trial. Pancreatic cancer patients who partake in clinical trials typically have more successful outcomes. Because there are only some approved chemotherapies and treatment options for pancreatic cancer, none that guarantee a cure, it is key to ask your doctor about what clinical trials may be available to you.
Doctors will often refer patients to clinical trials once all other approved therapies and options have been exhausted, or if they fit the criteria for a specific trial available. Clinical trials are essential in finding a cure to diseases like pancreatic cancer. They offer knowledge about cancers that we are still trying to understand as well as help find ways to detect cancer earlier and better improve a patient’s quality of life.
Once pancreatic cancer has spread beyond the pancreas chemotherapy or a combination of therapies is likely a patient’s best option. While many cancers have therapies that can eliminate tumors and allow remission, pancreatic cancer is not one of them.
Chemotherapy uses drugs, or a combination of drugs, to kill cancer cells by preventing their growth and division. It is important to note that while attacking the bad cells growing in your body, chemotherapy also affects the good cells. There are currently 4 FDA approved chemotherapies for pancreatic cancer considered to be the standard options, as well as some chemotherapies and combinations of therapies with such positive results that they are included as standard treatments.
Radiation is a localized therapy that uses high-energy waves or protons to kill cancer cells. It has been shown that radiation can prevent pancreatic tumors from growing further and at times shrink, but doctors often use radiation to aid with pain caused by a tumor or to keep an inoperable tumor from growing. Radiation is localized and unlike chemotherapy, it does not treat cancer cells that may be in other areas of the body. Radiation can similarly be given as neoadjuvant therapy (prior to surgery to reduce a tumor for easier removal) or adjuvant therapy (after surgery to target any cancer cells left behind). Radiation can be used alone but is often used in conjunction with chemotherapy.
Targeted therapies are drugs used to fight specific aspects of a cancer cell, causing less harm to healthy cells. Targeted treatments can be used in many ways and are specified to your individual tumor and cancer.
Immunotherapy fuels the immune system to attack the cancer from within. There are a number of benefits to immunotherapy such as slowing or stopping tumor growth however there is still much to learn about which patients benefit most from immunotherapy.